In the last few decades, research on probiotics has grown exponentially. Our understanding of how they can influence our gut health as well as how they influence seemingly unrelated systems such as the immune system has been greatly refined. Unfortunately, as research creates buzz, so does the marketing world and our shelves are popping up with probiotic labels everywhere. Now, we have a dilemma- how to decide which probiotics give you the bang for your buck. This current article builds on my last article explaining some of the research and the benefits of probiotics. If you haven’t read it you can check it out here.
Are all probiotics created equal?
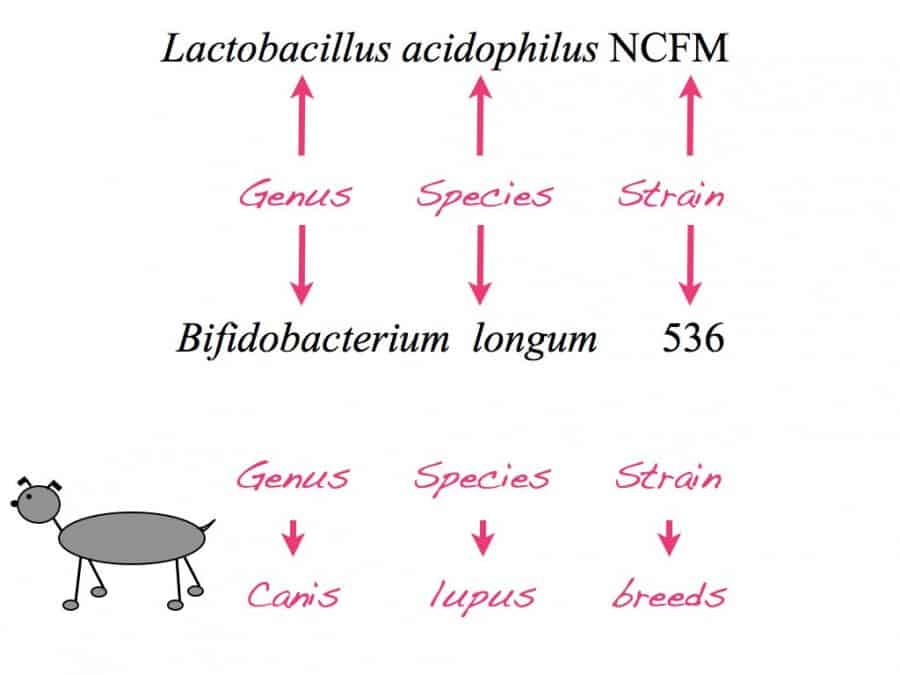
Saying I take probiotics is as vague as saying I take vitamins. Just as different vitamins play differing roles in the body, we also know that different probiotics with different genus, species and strains do not have the same effects.
If you currently take probiotics take a look at the label now.
What do you see? Can you find the Genus, species and strain of the probiotic?
Some of the lower quality probiotics only specify the genus and species and not the strain. This is because identifying strains take an additional level of evaluation. This step however is proving to be extremely important as we are learning that probiotics with the same genus and species but different strain can play different roles in your health and do not all confer the same benefits.
To conceptualize, consider that all dogs have the same genus and species- Canis lupus. Within this genus and species we have various types of dog breeds. Visually it is evident that different breeds have very different characteristics. For example, some are great hunter dogs others are better sled dogs while some are hypoallergenic dogs. Having a probiotic that doesn’t specify strain is like looking for a hunting dog but blindly buying a dog without knowing the breed.
Take home message: Top 5 things to know before choosing your probiotic
1. Know your probiotic strain
Look for a known probiotic strain that has been tested in humans and known to confer the specific outcome you are looking for.
2. Know the colony forming unit (CFU)
CFU indicates the amount of live microbes in the supplement. Recommending a dose is very difficult as it depends on the probiotic strain and the outcome you are looking for. Doses range from 50 million to 1 trillion CFU a day.
3. Know the probiotic strain’s tolerability to digestion.
Digestion provides a rough journey for some of these living microbes. Some strains are tough naturally and others aren’t. Has the strain you are taking been studied to assess its tolerability to the gastric acid of your stomach, the bile salts of your gallbladder and the digestives enzymes of your pancreas? Some strains are tolerant; some are not. The ones that aren’t need to be formulated in capsule that will only dissolve in the lower gastrointestinal track.
4. Know your manufacturer: 3 questions to ask.
Does this manufacturer ensure that strain-identification has been done, a process that ensures you have the strain of probiotic you are looking for? Is the manufacturer diligent about the entire process ensuring that if a probiotic needs to be refrigerated it is from the moment it leaves their hands, through shipment and until the time it gets to your home? Have they studied the probiotic to ensure it has a stable shelf life until expiry?
5. Are you having a double rainbow “what does it mean” moment?
I know, I’m sorry but it was a bit of the point of this article. I see so many patients taking probiotics but they have no idea what strain or for what outcome. Next time you see the word probiotic I hope you can see through some of the hype of what might be good marketing versus some of the benefits the best of science has to offer today. For overall intestinal and systemic health, the most basic recommendation in adults would be the periodic use of 15-30 billion of Lactobacillus acidophilus NCFM® (talk to your primary care giver). This strain was first isolated from the human gut and has been well researched. It is known to have digestive tolerability and been shown to adhere to the human intestinal wall. It is one of the most common probiotics in the gut and one with a very good safety record. There are over 6o studies on this specific strain demonstrating various beneficial outcomes for certain conditions.
Are you looking for specific outcomes, do you have irritable bowel syndrome or disease? If so, talking to someone who is well versed in the different strains of probiotics can get you inline with the research ensuring it has the best chance at improving the outcomes you are looking for.
If you would like more info, the International Scientific Association for Probiotics and Prebiotics (ISAPP) has been created to demystify some of complexities of this ever growing and expanding body of research. Hope you’ll have a more critical eye next time you see the word probiotic.